To download a copy of Claim Reconsideration-Appeal Process FAQ, click here.
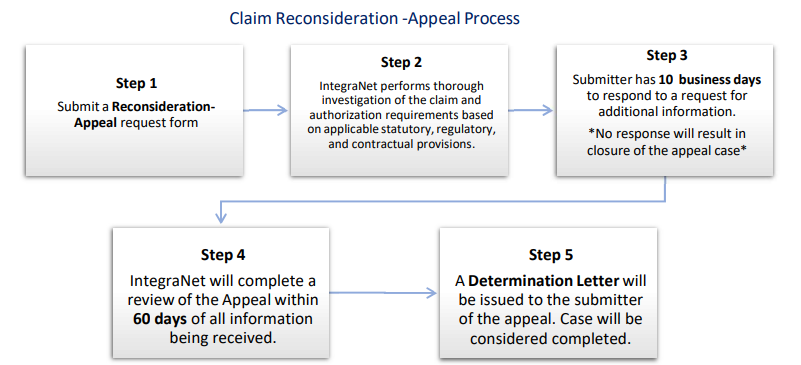
IntegraNet has established a unique Claims Appeal process that permits providers to dispute IntegraNet’s decisions for
claim denials.
This process addresses claim denials, including but not limited to:
Contracted providers must submit their request for Reconsideration to IntegraNet in accordance with their contract or within 120 calendar days from the date of the Explanation of Payment (EOP) when the contract does not specify a timeframe. Non- contracted providers must submit their request for Reconsideration within 60 calendar days from the date on the Explanation of Payment (EOP) along with a waiver of liability form is required for submission.
Two Methods of Appeal Submission |
|
|---|---|
| ELECTRONIC FORM | |
| Appeals & Grievances 2900 N. Loop West 7th Floor Houston, TX 77092 |
IntegraNet Claims Appeals/Reconsiderations |